A device for thoracic insufficiency syndrome that has been evolving for years is now more widely available
Thomas Morrow, MD

Thoracic
insufficiency syndrome (TIS) is a collection of rare disorders of the
thoracic skeletal system affecting about 4,000 newborns in the United
States each year. TIS may cause pulmonary failure because of decreased
lung volume: The ribs fuse together, the thoracic spine twists and
rotates, and the patient may slowly suffocate unless reconstruction is
done to multiple ribs and the spine, and is repeated as the child grows.
TIS is sometimes secondary to trauma. It may also be caused by
resection of large tumors from the chest wall and surgical separation of
conjoined twins.
Other cases are associated with well-defined genetic disorders and
disorders that are less well characterized from a genetic perspective
but also cause deformities of the bones in the thorax. These disorders
include constrictive chest wall syndrome; progressive congenital,
neurogenic, or idiopathic scoliosis without rib fusion; and hypoplastic
thorax syndrome, which includes Jeune’s syndrome, also called
asphyxiating thoracic dysplasia; Ellis-van Creveld syndrome, also called
mesoectodermal dysplasia, and Jarcho-Levine syndrome, which has gone by
nearly a dozen different names.
As you might imagine, the deformities can come in a wide variety of
forms because each of these conditions can affect the ribs and
individual vertebrae in different ways.
Early surgical interventions include fusion of the vertebrae to
prevent twisting and turning and insertion of custom manufactured
expandable instruments called “growing rods.”
The rib cage in children with TIS has a variety of missing, fused,
and deformed ribs. The fused ribs needed to be split apart and kept
apart with spacers. Missing ribs have been replaced with artificial ribs
of a fixed size or cadaver bone. In some cases, surgeons have resorted
to splitting the breastbone—anything to allow the lung space to expand,
not only for respiration but also growth of the child.

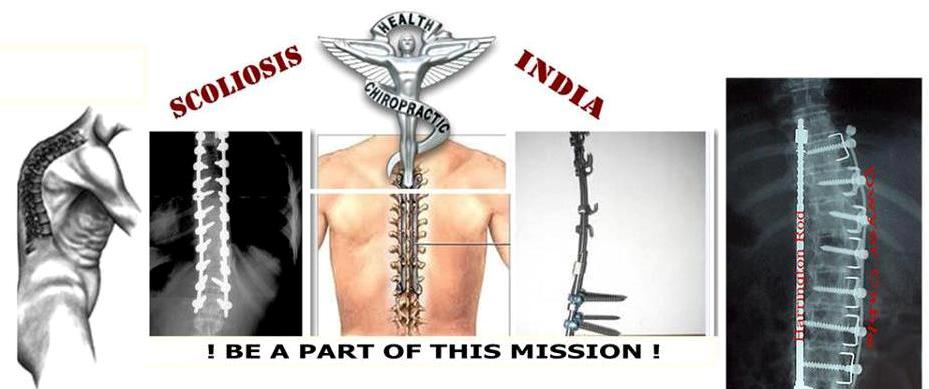
VEPTR device can be configured for rib-to-rib, rib-to-lumbar lamina, and rib-to-ilium (not pictured) attachment.
The Vertical Expandable Prosthetic Titanium Rib (VEPTR) addresses
many of the deformities of the rib cage and spine. The device was
developed by Robert Campbell Jr., MD, a surgeon at Children’s Hospital
of Philadelphia, who spent 25 years refining it. It consists of curved
titanium rods that are surgically attached to the ribs, lumbar vertebra,
or sacrum. VEPTR is perhaps the most configurable device ever approved
by the FDA. Because there is no standard presentation, any device for
the condition either needs to be entirely customized or capable of being
assembled, like parts of an erector set, to create a unique solution
for each child.
Increasing life expectancy
According to an FDA staff report, VEPTR is the only treatment
available that allows the chest cavity to be enlarged vertically,
providing room for the lungs to grow and improving the function of the
lungs and heart, thereby increasing the life expectancy of these
terminally ill children. The VEPTR is also unique because it treats the
deformities of both the spine and thorax. Moreover, it can be adjusted
through minor surgery as the child grows. Other devices need to be
replaced, and that often requires major surgery.
The FDA originally approved Campbell’s VEPTR device in 2004 under its
special humanitarian device exemption for conditions that affect small
numbers of people. Late last year, the agency gave the device 501(k)
clearance, which means it can now be used more widely.
The 501(k) clearance was based upon a single-arm, nonrandomized,
prospective multicenter trial done in two phases. The children served as
their own control because there is no “typical” pattern on which to
create a control group.
All subjects in the study were children six months or older, up to
the age of skeletal maturity, which is typically at 15–17 years of age.
The endpoints included increases in thoracic spinal height, hemithoracic
height and width, and scoliosis correction.
Because the patients are young and sometimes developmentally delayed,
standard pulmonary tests often can’t be done. This study used “assisted
ventilator rating” outcomes as an endpoint instead. Those ratings
reflect whether a child needs supplemental oxygen and other kinds of
assistance to breathe.
Because the 257 patients treated were growing, the study device would
periodically require expansion or replacement of its components. Each
child was expected to need many adjustments as a normal course of
treatment. Surgeons performed 1,538 surgical procedures during the
study’s 14 years. Twelve children died but in the opinion of the
investigators none of the deaths were related to the device.
The results can only be termed remarkable: 92% of the subjects
displayed either stabilization or improvement in a statistic called
assisted ventilator rating, which sums up indirect measurements of
pulmonary function and quality-of-life measurements. Radiographic
success was measured across four different types of deformity. Some of
the subgroups had 100% of patients reaching the predetermined goal. In
most of the 24 individual measures, more than 3 out of 4 of subjects
reached the goal.
Not all the studies of VEPTR have been positive. Last year, surgeons
at the University of Pittsburgh Medical Center reported that the forced
vital capacity of their VEPTR patients improved during six years of
follow-up but that it didn’t keep up with the child’s growth. They also
observed increased chest wall stiffness and increased thoracic kyphosis.
TIS is a life-threatening and, in some patients, a terminal condition
that almost without exception requires some sort of surgical
intervention. The previous static surgical treatments were unable to
adapt to the growing child’s needs. No prior treatments were able to
address the various deformities effectively. The development of the
VEPTR now provides the potential benefits of continued spinal growth,
decreased deformity, and improved breathing ability.
This device is the result of more than two decades of development and
is another example of how continual refinements over long periods of
time can lead to Tomorrow’s Medicine!
Thomas Morrow, MD, is chief medical officer of Next
IT. He is the immediate past president of the National Association of
Managed Care Physicians and has 24 years of managed care experience at
the payer or health plan level. The views expressed here are his alone.
Contact him at TMorrow@ManagedCareMag.com.
Source: Managed Care, Feb 2015
No comments:
Post a Comment