Spinal fusions, a surgery to permanently join together two or more vertebrae in the spine so there is no movement between them, are more common than they should be, says Elian M. Shepherd, M.D., FACS, Director of the Methodist Hospitals Spine Care Center and a board certified orthopedic surgeon, noting that he often has patients come to his office frightened and experiencing severe back pain.


Surgery on specific areas in the spinal column can result in pain relief as well as curbing degenerative effects of disease or injury.
“They might say to me I had an MRI and have three bulging disks, but none of that is important,” he says. That is not a sign for spinal fusion, it’s a sign of age,” he says. “Spinal fusion is needed when your spine is deformed, when people are bent over when they walk or the spine goes one way or the other.”
“They might say to me I had an MRI and have three bulging disks, but none of that is important,” he says. That is not a sign for spinal fusion, it’s a sign of age,” he says. “Spinal fusion is needed when your spine is deformed, when people are bent over when they walk or the spine goes one way or the other.”
And even then there are caveats. Spinal fusions can improve the quality of life but for the elderly there’s a risk involved as well.
“I tell them you need to have a fusion,” Shepherd says, “but I tell them they’re old and surgery at that age can be risky. So they go home and think about it and come back the next day and say I want to do it. I want to have a better quality of life.”
The spine, consists of 26 bone discs called vertebrae which protect the spinal cord and allow a person to stand and bend. Spine disorders, infections, tumors and traumatic injury often cause intense pain when bone changes put pressure on the spinal cord or nerves.
Think of spinal fusion as a type of high level welding where the surgeon fuses two or more painful vertebrae with the ultimate goal of healing them into one single, solid bone.
Spines are a complex system and so special consideration should be undertaken before going directly to surgery.
That’s why Shepherd frequently suggests physical therapy, pain medication and treatment with anti-inflamatories as well as always getting a second opinion before taking the next step.
“Spine surgery is not something to be decided in a week,” he says.
For those of us who think a spine is a spine, that’s not so.
“What’s normal for you is not normal for everyone,” Shepherd says.
We’re born with angles and alignments (which refers to how the head, shoulders, spine, hips, knees and ankles relate and line up with each other) in the spine, each in an individual way and which remain much the same, barring injury and other factors, throughout our lives.
Shepherd says it’s important for surgeons to know about these alignments and angels before performing a spinal fusion to avoid compounding the problem.
“We have a special x-ray that shows us the spine from the neck to the hip and then use software to measure the angles before we operate,” he says. “When we fuse the spine, it should look like the Eiffel Tower. “Not the Leaning Tower of Pisa.”
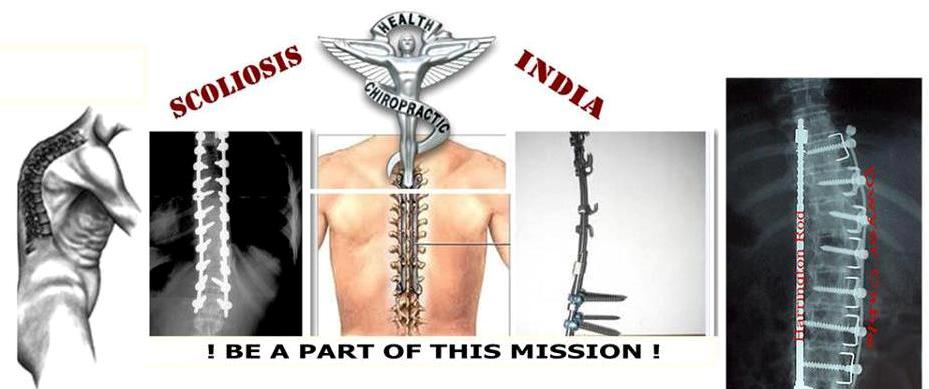
Spine fusions become necessary when the spine shows significant or worsening instability and deformity such as from scoliosis, “says Srinivasu Kusuma, MD, an orthopedic spine surgeon on staff at Ingalls Memorial Hospital. Scoliosis is condition where the spine curves sideways, frequently occurring during the growth spurt just before puberty. Though most spines have a slight but minute curvature, with scoliosis the spine curves too much to the point where it looks like the letters “C” or “S.”
“Spine fusions are not an uncommon procedure,” continues Kusuma. “As a spine surgeon, I see more than the average orthopedic surgeon.”
According to Kusuma, the most common causes of spinal fusions include trauma such as fractures or dislocations of the spine, degenerative instability like when arthritis causes one vertebrae to slip forward compared to the other vertebrae and scoliosis.
Source : nwitimes , 22nd oct 2014
Source : nwitimes , 22nd oct 2014
No comments:
Post a Comment